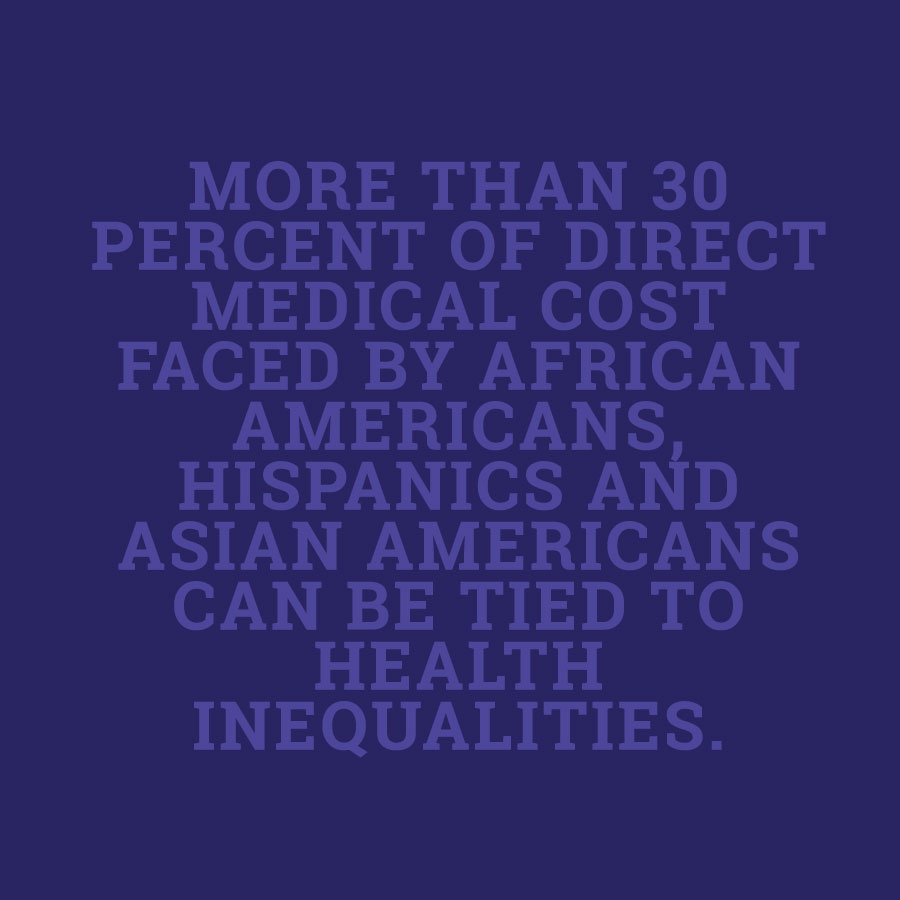
Because of inequitable access to care, these populations are sicker when they do find a source of care and incur higher medical costs. That 30 percent translates to more than $230 billion over a four-year period.

Nearly 84 million people live in an area with a shortage of healthcare providers. A shortage of 91,500 physicians is anticipated by 2020 within the United States. This number is expected to increase to over 130, 600 by 2025, significantly reducing overall access to care.

Race-concordant care produced longer visits; increased provider participation and communication; and higher ratings of client satisfaction and trust compared with race-discordant visits. Provider-client communication has been associated with commitment to care plans/medical instructions, client satisfaction and health outcomes resulting in greater quality of care.
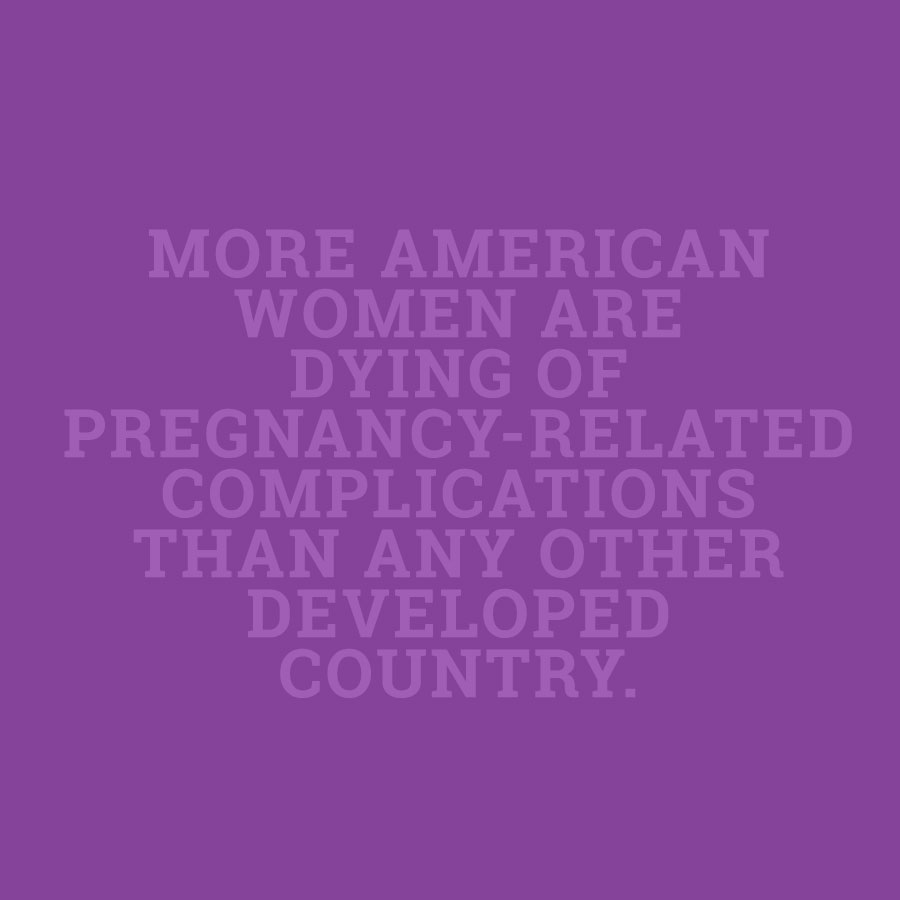
Only in the U.S. has the rate of women who die as a result of pregnancy related complications continued to rise. This rise is most significant among African Americans, who are 2 to 3 times more likely to die from pregnancy-related causes than their non-Hispanic, Caucasian counterparts. Further, African-American infants die at almost twice the rate of their white counterparts.
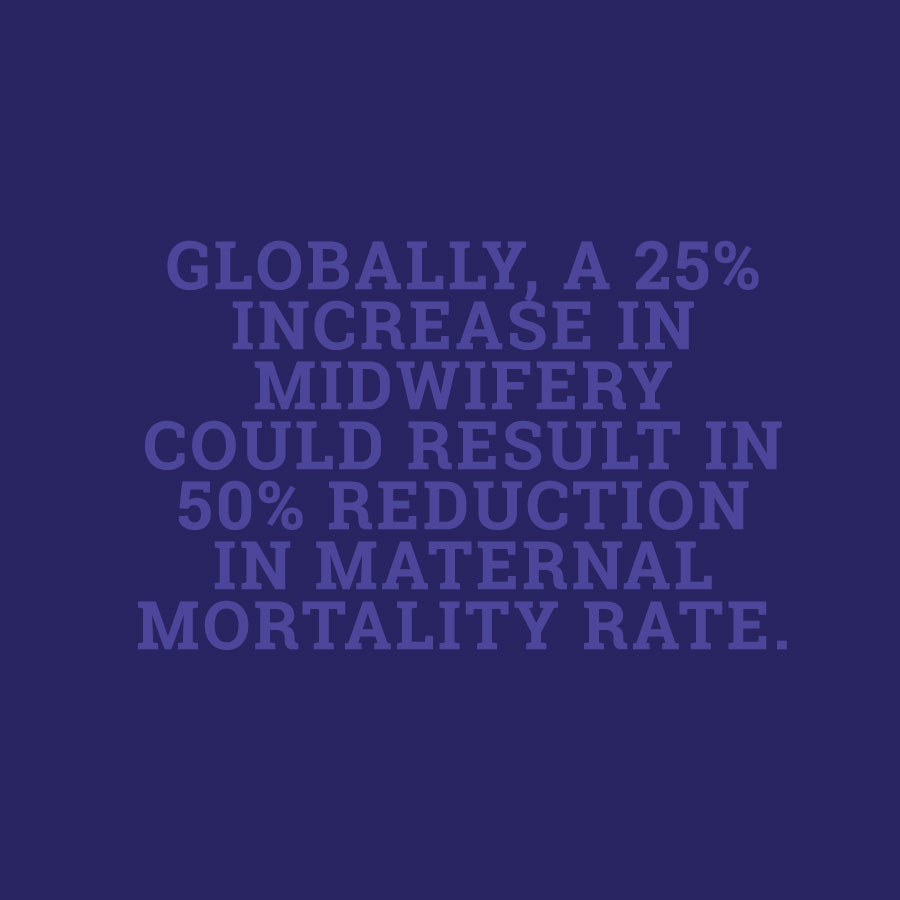
Though this projection is developed from a global perspective it is relevant for populations in the United States that lack adequate access to maternity care, specifically rural communities, low-income populations, and racial/ethnic minority groups. With the growing shortage of physicians and significant effects of women’s health care disparities, improving access to midwifery care is paramount.